
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- A Comparison of Predictive Performances between Old versus New Criteria in a Risk-Based Screening Strategy for Gestational Diabetes Mellitus
- Subeen Hong, Seung Mi Lee, Soo Heon Kwak, Byoung Jae Kim, Ja Nam Koo, Ig Hwan Oh, Sohee Oh, Sun Min Kim, Sue Shin, Won Kim, Sae Kyung Joo, Errol R. Norwitz, Souphaphone Louangsenlath, Chan-Wook Park, Jong Kwan Jun, Joong Shin Park
- Diabetes Metab J. 2020;44(5):726-736. Published online April 13, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0126
- 6,599 View
- 123 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background The definition of the high-risk group for gestational diabetes mellitus (GDM) defined by the American College of Obstetricians and Gynecologists was changed from the criteria composed of five historic/demographic factors (old criteria) to the criteria consisting of 11 factors (new criteria) in 2017. To compare the predictive performances between these two sets of criteria.
Methods This is a secondary analysis of a large prospective cohort study of non-diabetic Korean women with singleton pregnancies designed to examine the risk of GDM in women with nonalcoholic fatty liver disease. Maternal fasting blood was taken at 10 to 14 weeks of gestation and measured for glucose and lipid parameters. GDM was diagnosed by the two-step approach.
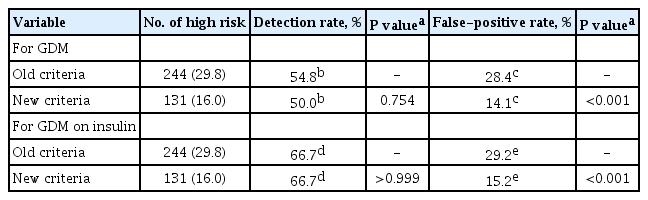
Results Among 820 women, 42 (5.1%) were diagnosed with GDM. Using the old criteria, 29.8% (
n =244) of women would have been identified as high risk versus 16.0% (n =131) using the new criteria. Of the 42 women who developed GDM, 45.2% (n =19) would have been mislabeled as not high risk by the old criteria versus 50.0% (n =21) using the new criteria (1-sensitivity, 45.2% vs. 50.0%,P >0.05). Among the 778 patients who did not develop GDM, 28.4% (n =221) would have been identified as high risk using the old criteria versus 14.1% (n =110) using the new criteria (1-specificity, 28.4% vs. 14.1%,P <0.001).Conclusion Compared with the old criteria, use of the new criteria would have decreased the number of patients identified as high risk and thus requiring early GDM screening by half (from 244 [29.8%] to 131 [16.0%]).
-
Citations
Citations to this article as recorded by- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2023; 38(1): 129. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Subsequent Development of Adverse Pregnancy Outcomes
Seung Mi Lee, Young Mi Jung, Eun Saem Choi, Soo Heon Kwak, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Bo Kyung Koo, Sue Shin, Errol R. Norwitz, Chan-Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Clinical Gastroenterology and Hepatology.2022; 20(11): 2542. CrossRef - Nonalcoholic fatty liver disease and early prediction of gestational diabetes mellitus using machine learning methods
Seung Mi Lee, Suhyun Hwangbo, Errol R. Norwitz, Ja Nam Koo, Ig Hwan Oh, Eun Saem Choi, Young Mi Jung, Sun Min Kim, Byoung Jae Kim, Sang Youn Kim, Gyoung Min Kim, Won Kim, Sae Kyung Joo, Sue Shin, Chan-Wook Park, Taesung Park, Joong Shin Park
Clinical and Molecular Hepatology.2022; 28(1): 105. CrossRef - Nonalcoholic fatty liver disease-based risk prediction of adverse pregnancy outcomes: Ready for prime time?
Seung Mi Lee, Won Kim
Clinical and Molecular Hepatology.2022; 28(1): 47. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
Diabetes & Metabolism Journal.2022; 46(4): 605. CrossRef - Development of early prediction model for pregnancy-associated hypertension with graph-based semi-supervised learning
Seung Mi Lee, Yonghyun Nam, Eun Saem Choi, Young Mi Jung, Vivek Sriram, Jacob S. Leiby, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan-Wook Park, Jong Kwan Jun, Won Kim,
Scientific Reports.2022;[Epub] CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - The risk of pregnancy‐associated hypertension in women with nonalcoholic fatty liver disease
Young Mi Jung, Seung Mi Lee, Subeen Hong, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan‐Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Liver International.2020; 40(10): 2417. CrossRef
- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
- Effects of Resistance Training and Aerobic Exercise on Insulin Sensitivity in Overweight Korean Adolescents: A Controlled Randomized Trial
- Sunghwan Suh, In-Kyong Jeong, Mi Yeon Kim, Yeon Soo Kim, Sue Shin, Sun Sin Kim, Jae Hyeon Kim
- Diabetes Metab J. 2011;35(4):418-426. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.418
- 21,480 View
- 46 Download
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Data on the impact of resistance training on insulin resistance in overweight or obese children are inconclusive.
Methods Thirty overweight South Korean adolescents (mean age of 13.10 years) were divided by sex, and then randomly assigned to one of three treatment groups, which were the diet only (DO), diet with aerobic exercise (AE), or diet with resistance training (RT) group. Physiologic and metabolic parameters were assessed at baseline and after 12 weeks of exercise training and diet modification.
Results Both exercise groups (aerobic and resistance) showed significant improvements in their insulin area under the curve and insulin sensitivity index values when compared to their baseline values while the DO group showed no significant changes in these variables. Age-, sex-, and body mass index (BMI)-adjusted intergroup comparison analyses showed a marked reduction in BMI and a significant reduction in muscle mass in the AE group when compared to the RT group and the DO group, respectively.
Conclusion A 12-week exercise training program of either resistance or aerobic activity improved insulin sensitivity in overweight adolescents, although it failed to show superiority over a DO program. Aerobic exercise decreased both body weight and BMI, and it was noted that this group also had a significant reduction in muscle mass when compared to the DO group.
-
Citations
Citations to this article as recorded by- Effect of high-intensity interval training and moderate-intensity continuous training on cardiovascular risk factors in adolescents: Systematic review and meta-analysis of randomized controlled trials
Ya Wang, Shun Wang, Xiangwu Meng, Husheng Zhou
Physiology & Behavior.2024; 275: 114459. CrossRef - Exercise and Nutrition Strategies for Combating Sarcopenia and Type 2 Diabetes Mellitus in Older Adults
Dionysia Argyropoulou, Nikolaos D. Geladas, Tzortzis Nomikos, Vassilis Paschalis
Journal of Functional Morphology and Kinesiology.2022; 7(2): 48. CrossRef - Effects and dose-response relationships of exercise intervention on weight loss in overweight and obese children: a meta-regression and system review
Rui Xu, Qiao-Ting Huang, Yu-Ting Chen, Peng-Yin Wang
Journal of Pediatric Endocrinology and Metabolism.2022; 35(9): 1117. CrossRef - The Benefits of Resistance Training in Obese Adolescents: A Systematic Review and Meta-analysis
Bruno Ribeiro, Pedro Forte, Raquel Vinhas, Daniel A. Marinho, Luís B. Faíl, Ana Pereira, Fernando Vieira, Henrique P. Neiva
Sports Medicine - Open.2022;[Epub] CrossRef - Effects of Eight Weeks of Combined Training with Antioxidant Vitamins E and C on Glutathione, Glutathione Peroxidase, and Superoxide Dismutase in the Heart Tissue of Streptozotocin-induced Diabetic Rats
Elaheh Heydarnia, Farzaneh Taghian, Khosro Jalali Dehkodi, Mehrzad Moghadasi
Gene, Cell and Tissue.2021;[Epub] CrossRef - Effect of resistance training with and without caloric restriction on visceral fat: A systemic review and meta‐analysis
Mousa Khalafi, Abbas Malandish, Sara K. Rosenkranz, Ali A. Ravasi
Obesity Reviews.2021;[Epub] CrossRef - IMPACT OF TREADMILL RUNNING ON BLOOD GLUCOSE LEVEL OF TYPE 2 DIABETES MELLITUS PATIENTS IN GHURKI TRUST AND TEACHING HOSPITAL
Samiya Noreen, Muhammad Shafique, Tayyaba Mustafa Mian, Hafiz Abdul Rehman, Abdul Rehman, Muhammad Saad Shafiq, Ibraheem Zafar, Ramsha Masood
Pakistan BioMedical Journal.2021;[Epub] CrossRef - Role of exercise on insulin sensitivity and beta-cell function: is exercise sufficient for the prevention of youth-onset type 2 diabetes?
Joon Young Kim, Justin Y. Jeon
Annals of Pediatric Endocrinology & Metabolism.2020; 25(4): 208. CrossRef - Effects of HIIT and MICT on cardiovascular risk factors in adults with overweight and/or obesity: A meta-analysis
LiQiang Su, JinMei Fu, ShunLi Sun, GuangGao Zhao, Wei Cheng, ChuanChuan Dou, MingHui Quan, Belinda Parmenter
PLOS ONE.2019; 14(1): e0210644. CrossRef - What Is the Role of Resistance Exercise in Improving the Cardiometabolic Health of Adolescents with Obesity?
SoJung Lee, YoonMyung Kim, Jennifer L. Kuk
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 76. CrossRef - Does exercise training affect resting metabolic rate in adolescents with obesity?
Angela S. Alberga, Denis Prud’homme, Ronald J. Sigal, Gary S. Goldfield, Stasia Hadjiyannakis, Réjeanne Gougeon, Penny Phillips, Janine Malcolm, George A. Wells, Steve Doucette, Jinhui Ma, Glen P. Kenny
Applied Physiology, Nutrition, and Metabolism.2017; 42(1): 15. CrossRef - Iniciación al entrenamiento de fuerza en edades tempranas: revisión
G. Peña, J.R. Heredia, C. Lloret, M. Martín, M.E. Da Silva-Grigoletto
Revista Andaluza de Medicina del Deporte.2016; 9(1): 41. CrossRef - Effects of aerobic training, resistance training, or both on cardiorespiratory and musculoskeletal fitness in adolescents with obesity: the HEARTY trial
Angela S. Alberga, Denis Prud’homme, Ronald J. Sigal, Gary S. Goldfield, Stasia Hadjiyannakis, Penny Phillips, Janine Malcolm, Jinhui Ma, Steve Doucette, Rejeanne Gougeon, George A. Wells, Glen P. Kenny
Applied Physiology, Nutrition, and Metabolism.2016; 41(3): 255. CrossRef - The response of circulating omentin-1 concentration to 16-week exercise training in male children with obesity
Farzad Zehsaz, Negin Farhangi, Mehri Ghahramani
The Physician and Sportsmedicine.2016; 44(4): 355. CrossRef - Epidemiology of Childhood Obesity in Korea
Kyoung Hwa Ha, Dae Jung Kim
Endocrinology and Metabolism.2016; 31(4): 510. CrossRef - Muscle strength in youth and cardiovascular risk in young adulthood (the European Youth Heart Study)
Anders Grøntved, Mathias Ried-Larsen, Niels Christian Møller, Peter Lund Kristensen, Karsten Froberg, Søren Brage, Lars Bo Andersen
British Journal of Sports Medicine.2015; 49(2): 90. CrossRef - Position statement on youth resistance training: the 2014 International Consensus
Rhodri S Lloyd, Avery D Faigenbaum, Michael H Stone, Jon L Oliver, Ian Jeffreys, Jeremy A Moody, Clive Brewer, Kyle C Pierce, Teri M McCambridge, Rick Howard, Lee Herrington, Brian Hainline, Lyle J Micheli, Rod Jaques, William J Kraemer, Michael G McBride
British Journal of Sports Medicine.2014; 48(7): 498. CrossRef - Abdominal obesity and low physical activity are associated with insulin resistance in overweight adolescents: a cross-sectional study
Claudia-María Velásquez-Rodríguez, Marcela Velásquez-Villa, Leidy Gómez-Ocampo, Juliana Bermúdez-Cardona
BMC Pediatrics.2014;[Epub] CrossRef - Exercise and Insulin Resistance in Youth: A Meta-Analysis
Michael V. Fedewa, Nicholas H. Gist, Ellen M. Evans, Rod K. Dishman
Pediatrics.2014; 133(1): e163. CrossRef - What is the Effect of Resistance Training on the Strength, Body Composition and Psychosocial Status of Overweight and Obese Children and Adolescents? A Systematic Review and Meta-Analysis
Natasha Schranz, Grant Tomkinson, Tim Olds
Sports Medicine.2013; 43(9): 893. CrossRef - A Review of Randomized Controlled Trials of Aerobic Exercise Training on Fitness and Cardiometabolic Risk Factors in Obese Adolescents
A. S. Alberga, A. Frappier, R. J. Sigal, D. Prud'homme, G. P. Kenny
The Physician and Sportsmedicine.2013; 41(2): 44. CrossRef - Effects of Aerobic Versus Resistance Exercise Without Caloric Restriction on Abdominal Fat, Intrahepatic Lipid, and Insulin Sensitivity in Obese Adolescent Boys
SoJung Lee, Fida Bacha, Tamara Hannon, Jennifer L. Kuk, Chris Boesch, Silva Arslanian
Diabetes.2012; 61(11): 2787. CrossRef
- Effect of high-intensity interval training and moderate-intensity continuous training on cardiovascular risk factors in adolescents: Systematic review and meta-analysis of randomized controlled trials

 KDA
KDA
 First
First Prev
Prev





